Overview
The American Academy of Pediatrics (AAP) has published and updated evidence-based guidelines for managing hyperbilirubinemia in newborns who are at least 35 weeks gestation1,2.
Infants less than 35 weeks gestation are believed to be at greater risk for bilirubin-associated brain damage than term infants, but there is inadequate data to guide evidence-based practice. In 2012, expert consensus-based guidelines were developed for guiding management of hyperbilirubinemia in preterm infants3, and a web-based tool (Premie BiliRecs, Stanford Medicine Children’s Health) was developed to provide clinical decision support (CDS)4–6.
At my institution, there has been increasing use of Premie BiliRecs. To provide partial integration with our electronic health record (EHR) and to facilitate large-scale analysis, I developed code to recreate the recommendations of Premie BiliRecs.
Regeneration of clinical decision thresholds
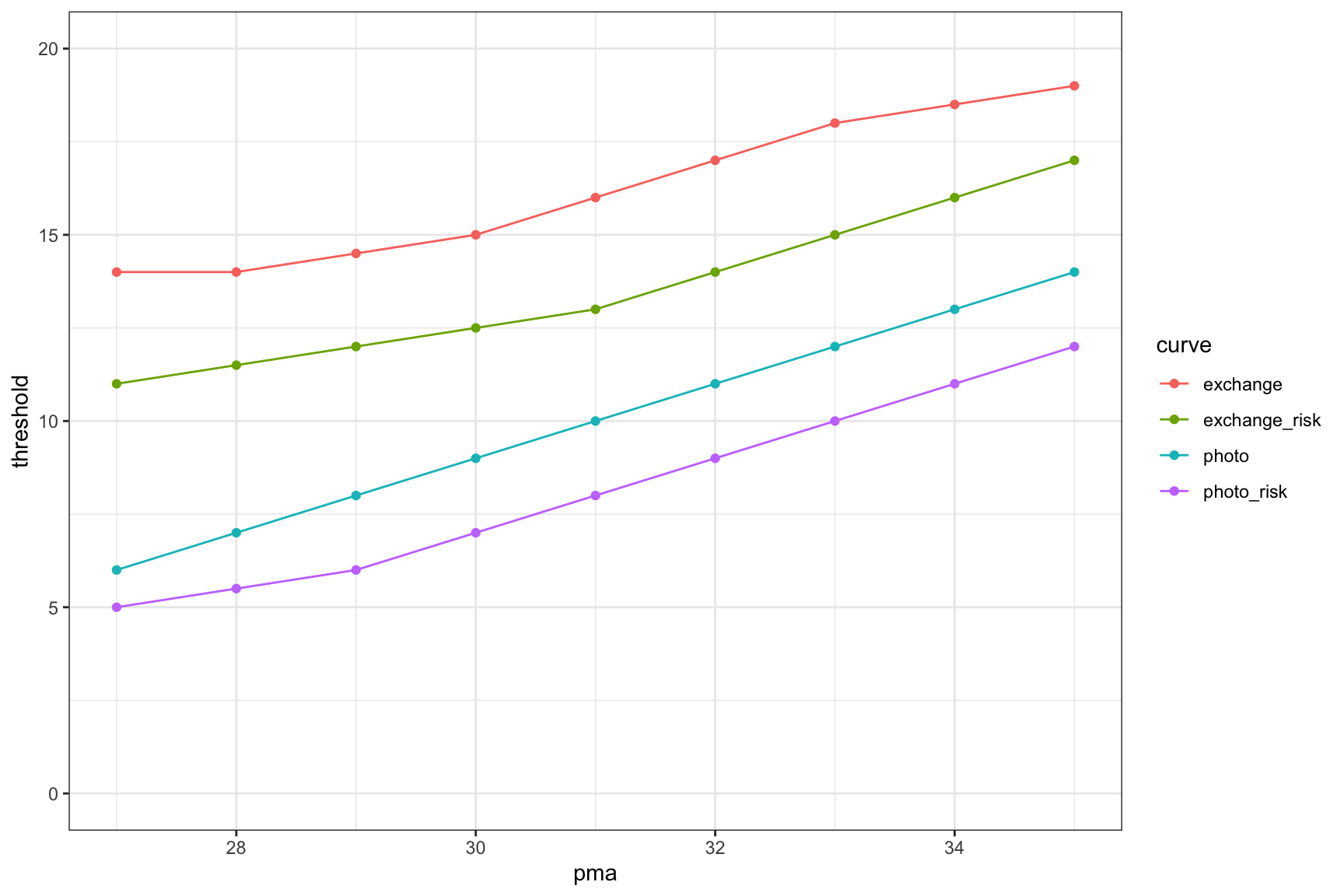
Published references4,5 and inspection of the online Premie Bilirecs web tool suggested that linear interpolation between a limited number number of points would be sufficient to regenerate the decision thresholds:
| pma | photo | photo_risk | exchange | exchange_risk |
|---|---|---|---|---|
| 27 | 6.0 | 5.0 | 14.0 | 11.0 |
| 28 | 7.0 | 5.5 | 14.0 | 11.5 |
| 29 | 8.0 | 6.0 | 14.5 | 12.0 |
| 30 | 9.0 | 7.0 | 15.0 | 12.5 |
| 31 | 10.0 | 8.0 | 16.0 | 13.0 |
| 32 | 11.0 | 9.0 | 17.0 | 14.0 |
| 33 | 12.0 | 10.0 | 18.0 | 15.0 |
| 34 | 13.0 | 11.0 | 18.5 | 16.0 |
| 35 | 14.0 | 12.0 | 19.0 | 17.0 |
Plotting lines connecting the points looked promising:
And finally, the derived lines were plotted directly over the graphic from the Premie Bilirecs website and matched well.
A close inspection of the graphic on Premie BiliRecs shows that all of their color ribbon total serum bilirubin decision threshold boundaries appear to be shifted up by 0.1 mg/dL compared with their own numeric decision thresholds. On the overlay plot generated here, I have also shifted the lines up by 0.1 mg/dL to match what their graphic displays.
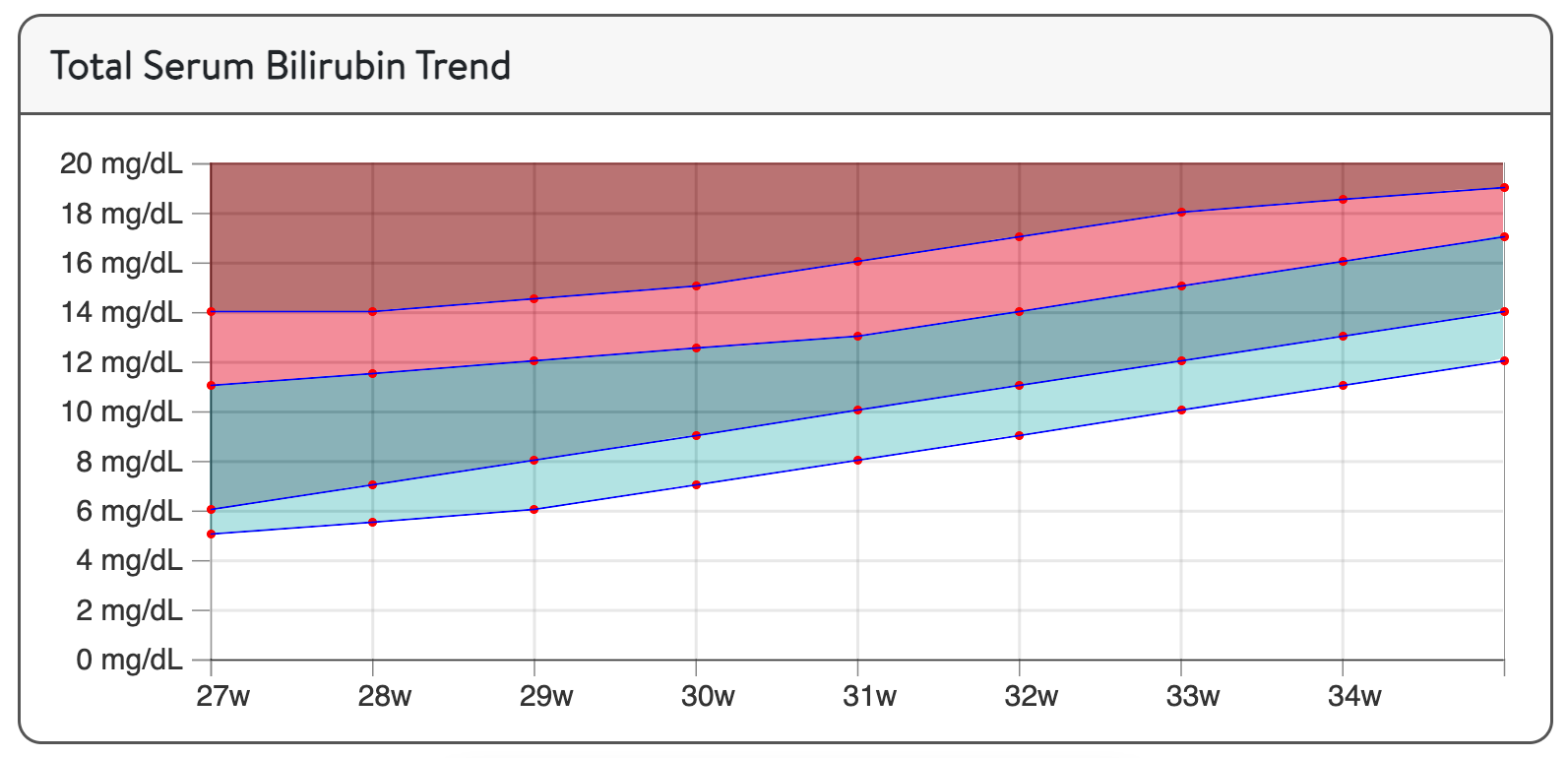
(from Premie BiliRecs)
Partial integration with the electronic health record
My institution uses the Epic EHR. Although I’ve been unsuccessful having tools directly integrated into the EHR, Epic does allow design of “SmartPhrases” and “SmartLinks” to populate text output including date of birth, gestational age at birth, and time + date of total serum bilirubin measurements.
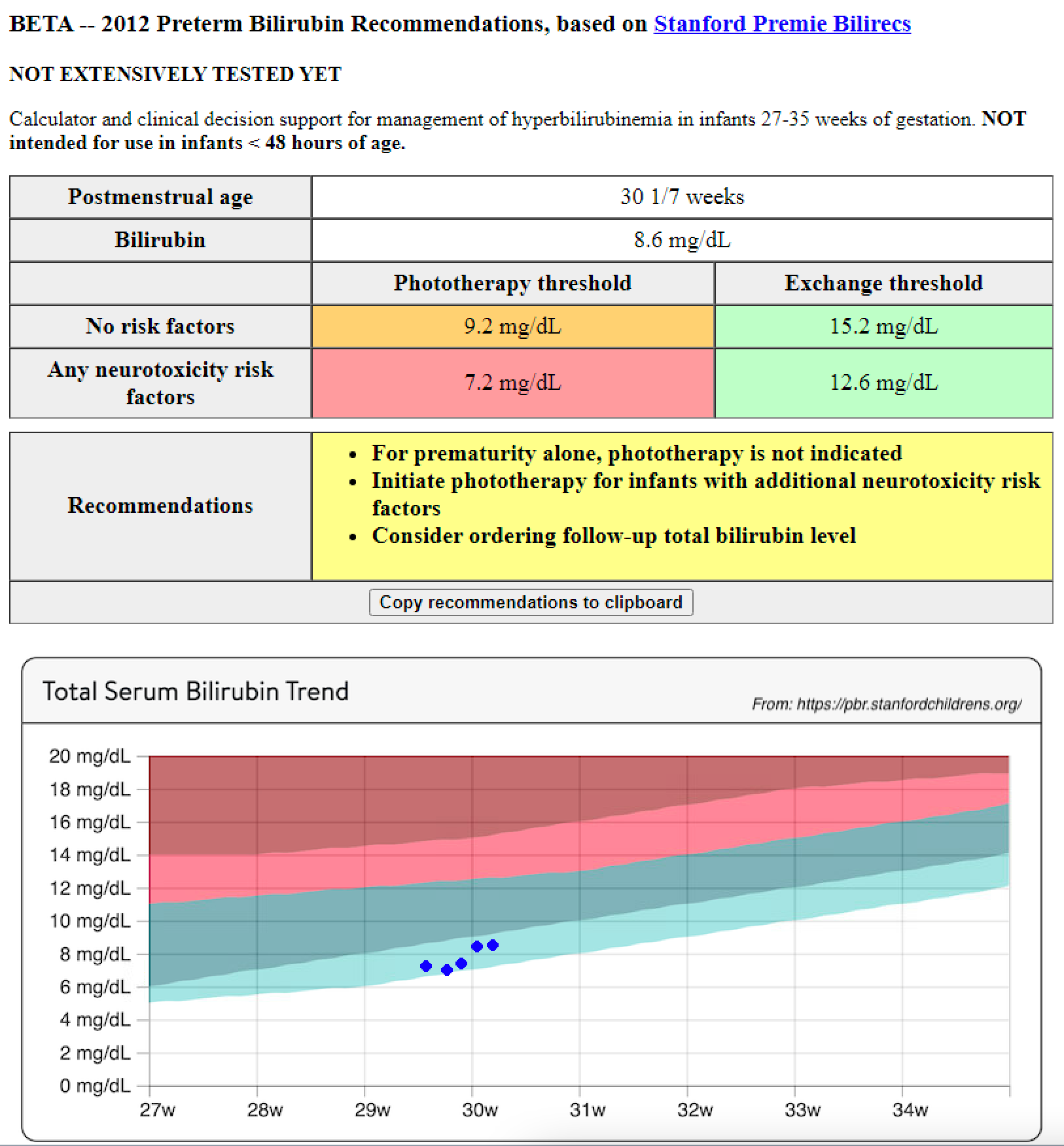
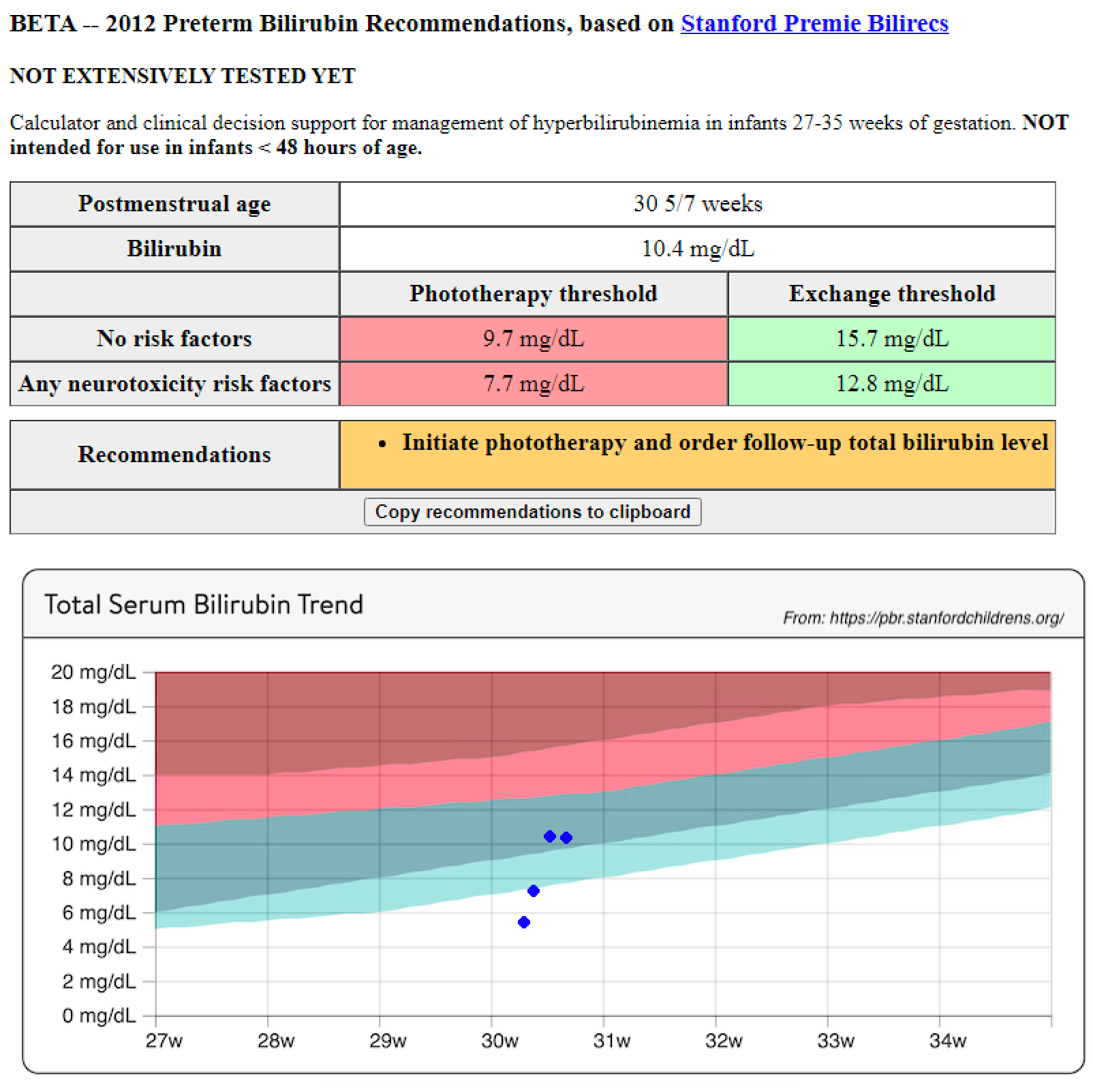
I designed an private, internal webtool that would take the output of a properly designed SmartPhrase to automate data entry and allow plotting of multiple bilirubin measurements and provide clinical decision support recommendation on the most recent measurement, based on the Premie BiliRecs recommendations. Example output follows:
Example 1: Slow rate-of-rise
Here’s an example of a gradual rate of rise, for which phototherapy might be avoided, so long as there were no neurotoxicity risk factors present.
Example 2: Rapid rate-of-rise; phototherapy started
Here’s an example of a clinically concerning rapid rate of rise, appropriately managed with phototherapy initiation.
Final thoughts and concerns
Although I’ve been aware of the Maisels 20123 expert consensus-based guidelines for quite some time, until recently I had not strictly followed them because they weren’t “official” (i.e., AAP-sanctioned) evidence-based clinical practice guidelines.
However, the increasing number of local clinicians using these guidelines has essentially made these the de facto standard, so I thought I should look more closely to better understand their intended use, as well as make it easier to follow the recommendations and potentially to large-scale analysis of local practice.
Caveats worth mentioning
One caveat is that age after birth should be more than 48 hours, which many clinicians appear to forget when using Premie BiliRecs.
The decision thresholds are significantly higher than those generated by other means.
For example, another guideline is to initiate phototherapy at a TSB (in mg/dL) of the current weight (in grams) divided by 200, and to consider exchange transfusion at twice that:
- i.e., a 1000 gram baby would have phototherapy started at 5 mg/dL and consider exchange at 10 mg/dL
- 1000 grams would be 50th percentile for a boy at 27 3/7 weeks, for which the (no risk factor) Premie BiliRecs phototherapy threshold would be 6.4 mg/dL (higher than 5 mg/dL)
Because of this, it may be more important to recognize when neurotoxicity risk factors might be present
Neurotoxicity risk factors that might be overlooked
A number of recommended neurotoxicity risk factors may not be obvious to those used to the 2004 and 2022 AAP guidelines for term or near-term infants. Some that I think might be easy to miss include:
- current intubation
- apnea or desaturation episode requiring PPV intervention
- albumin of < 2.5 g/dL (we don’t always routinely check albumin by 48 hours of age)
Routine use of the Stanford PremieBilirecs guidelines should adhere to their recommended usage.
EHR semi-integration
The local EHR increments the PMA by calendar date, which is convenient but not sensible.
For example, a baby born at 28 0/7 weeks at 11:59 pm will have their age incremented by a full day by 2 minutes after birth. This would also cause loss of precision when plotting multiple bilirubin measurements obtained on the same calendar date at different times.
I have instead opted for calculating the PMA smoothly, by calculating the precise age each bilirubin measurement was obtained and adding that to the initial birth gestation, irrespective of calendar date.
Anyway, just some thought as I consider personally implementing this practice change.
References
Footnotes
“Family Planning and Newborn Care” by The Global Financing Facility is licensed under CC BY-NC-ND 2.0.↩︎
